Mother/Infant Opioid Substance Use Treatment and Recovery Effort (MOSTaRE)
Interested in Getting Involved?
Need More Info?
Contact:
ella.rusnacko@minnesotaperinatal.org
Contact:
ella.rusnacko@minnesotaperinatal.org

- December 12th, 2024
- January 9th, 2025
- February 13th, 2025
- March 13th, 2025
- April 10th, 2025
- May 8th, 2025
- June 12th, 2025
- July 10th, 2025
- August 14th, 2025
- September 11th, 2025
- October 9th, 2025
MOSTaRE Cohort 1
These are a variety of resources provided by MPO/MNPQC and other organizations for healthcare providers and the public. Many links are provided by other organizations and are subject to change without notice.
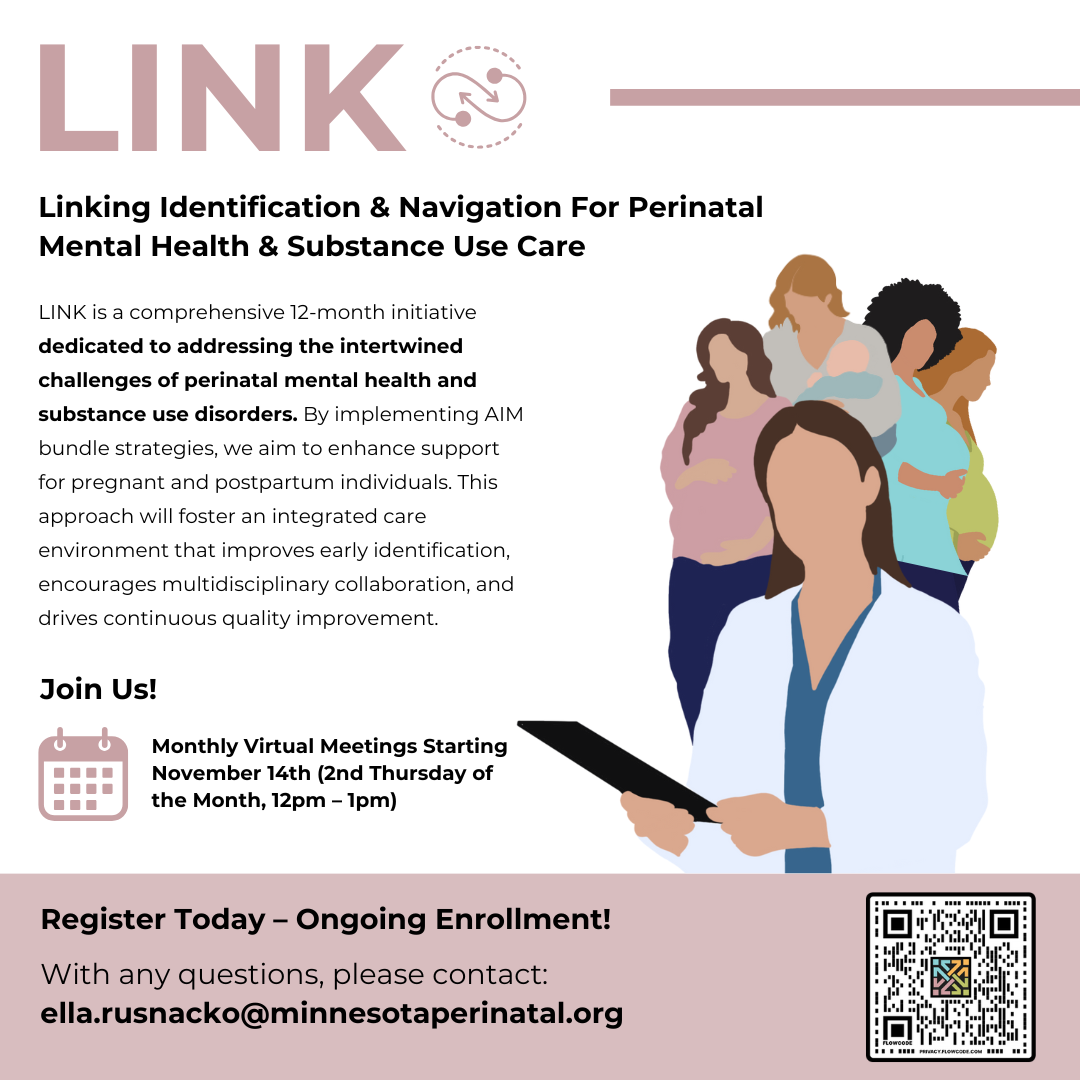
LINK Initiative
AIM
By December 2023, our aim is to increase the identification and treatment of substance use disorders (SUDs) in pregnant people and substance exposure in infants by 50% or more in order to improve pregnancy and postpartum outcomes, increase the use of non-pharmacologic methods for treating infants exposed to opioids and reduce the average length of stay for these infants.
Charter
The Mother/Infant Opioid and Substance use Treatment and Recovery Effort (MOSTaRE) purpose is to work with providers, hospitals, and other stakeholders to improve identification, clinical care, and coordinated treatment/support for pregnant and parenting individuals with opioid use disorder and their infants through a family-centered care approach.
The MOSTaRE Initiative will emphasize family-centered care that maintains the dyad and will address treatment and prevention of substance exposure during and after pregnancy for both mother and infant.
Team Membership (includes both infant/perinatal arms)
- Infant Team Members include: NICU, general pediatric or family practice provider, community treatment and support partners, women with lived experience
- Perinatal Team Members include: prenatal, delivery, and postpartum providers; treatment and community support members, women with lived experience
Family Of Measures
Stratify by race/ethnicity where available.
State Surveillance:
- SUD among pregnant and postpartum people (SS1)
- Severe Maternal Morbidity (SMM) (including transfusion codes) among people with SUD (SS2)
- Severe Maternal Morbidity (SMM) (excluding transfusion codes) among people with SUD (SS3)
- Proportion of pregnancy associated deaths due to overdose (SS4)
Outcome Measures:
- Percent of newborns exposed to substances in utero who were discharged to either birth parent (O1)
- Percent of pregnancy and postpartum people who received or were referred to recovery treatment services (O3)
- Length of stay of all opioid exposed newborns
Process Measures:
- Percent of pregnant and postpartum people screened for SUDs (P1)
- Number of Provider and Nursing education-SUDs (P5)
- Number of Provider and Nursing education- Respectful and Equitable Care (P6)
Structure Measures:
- Resource Mapping/ Identification of Community Resources (S1)
- Number of Patient Event Debriefs (S2)
- General Pain Managment Guidelines (S3)
- OUD Pain Managment Guidelines (S4)
- Validated Screening Tools and Resources Shared with Prenatal Care Sites (S5)
Resources
Behavioral Health Planning Council MDH
Drug & Alcohol Rehabs in Minnesota
Fast-Tracker – substance use disorder programs & resources
Fond du Lac Band of Lake Superior Chippewa
Hazelden Betty Ford Foundation
Hope House of Itasca County, Inc.
Minnesota Suboxone Providers & Doctors
Proof Alliance (formerly MOFAS)
Recovering Hope Treatment Center
Recovery-friendly Family-centered Pediatrics
St. Cloud Hospital/CentraCare Health
Specialized Treatment Services
Tribal and Urban Resources for Native Americans in Minnesota
Wayside Recovery Center
Perinatal Substance Use & Reporting Laws
Presented by Dr. Cresta Jones, MD, FACOG
March 2022
MNPQC Townhall
Response to changes in reporting of Prenatal Exposure to Controlled Substances
CPS Panel featuring Hennepin, Ramsey, Anoka,
and Beltrami County
May 11, 2022
Faculty
Working Group
MPH, Minnesota Department of Health,
Anne Walaszek, MPH (Anishinaabe) is the Maternal and Child Health Quality Improvement Specialist in the Women and Infant Health Unit at the Minnesota Department of Health. In her role, she leads two quality improvement grants, the Perinatal Quality Collaborative and the Communities Collaborating to Prevent Girls Opioid Abuse. Ms. Walaszek has experience working at a national non-profit addressing cancer inequities within American Indian and Alaska Native communities. In this role, she provided leadership for a clinic and community health approach to develop and implement culturally tailored evidence-based interventions to effectively build capacity in health systems across Indian Country. Her public health experience reflects grant writing, program development, research and data management throughout her experiences at the Minnesota Department of Health Diabetes Program, Institute of Child Development at the University of Minnesota, and SAMHSA for their Child, Adolescent and Family Branch. She is a 2017 recipient of the Lou Fuller Award for Distinguished Service in Eliminating Health Disparities.
Jane Taylor is an Improvement Advisor and Learning Designer. She supports learning collaboratives and innovation projects by providing expertise in improvement approaches and measurement. Since 2016, Jane has provided quality improvement expertise for MN Perinatal Association and MNPQC on Preventing Preterm Births, Hypertension in Pregnancy and Postpartum Care, The Early Hearing Diagnosis Initiatives, and the MOSTaRE Opioid Project. Currently she severs on the Data Committee and the Steering Committee.
Jane has dedicated the last 22 years of her profession career to improving lives for newborns, infants, children and birthing people. For fun she is an amateur violinist and ballroom competitor. She enjoys sailing on Lake Pepin in the summer with her husband and their dog, Pepper.
BSN, MS, RN, MPO/MNPQC Executive Director
Susan has been a Clinical Nurse Specialist in Women’s Health for over 30 years. She has a long history with MPO as a volunteer, conference presenter, planning committee member, and has served on the Board of Directors. She is currently the MPO Executive Director and Co-Director of the Minnesota Perinatal Quality Collaborative (MNPQC).
She enjoys the outdoors, hiking and kayaking, and loves the solitude of their cabin in the Boundary Waters.
MD, Ob/GYN | HealthPartners
I am continuously grateful that I have chosen a career in obstetrics and gynecology. I have the wonderful variety of labor and delivery, surgery and clinical care. My patients range in age from adolescence to menopause and they’ve all taught me so much about life. I have special interests in colposcopy and cervical procedures, high-risk obstetrics and vaginal surgery. I offer minimally invasive surgery whenever possible and perform many procedures in the clinic setting. My philosophy is that well-informed patients make the best medical decisions, so counseling regarding contraception, menopause and bleeding issues is an important part of my practice.
DNP, RN, PHNA-BC, Minnesota Department of Health
I’m a precise, thoughtful Doctor of Nursing with a passion for impacting population health. I was recently named a 2017 American Nurse Association “40 under 40” Emerging Nurse Leader.
I’m driven to identify public health issues and gaps and work with communities to design and implement solutions to address health equity. As a CBPR proponent with a variety of research methods experience, I have an understanding of Chicago-area communities and resources. I’m able to leverage the skills and expertise of peers and co-leaders to ensure desired outcomes. I’m adept with operational management and fiscal concerns and able to find cost-savings and efficiencies while maintaining staff satisfaction. I’m highly valued for being analytical and data-savvy. I lead interdisciplinary teams to improve quality of care. I’m a systems thinker who works toward policy development and change to benefit communities.
BSN, RN, DNP
Alison is a Women’s Health Gender-Related Nurse Practitioner Student the University of Minnesota
MD, PhD, Hennepin Health
I am passionate about providing you and your loved ones with the most evidence-based, compassionate care available to improve your health. I want to meet you where you are today, and help you improve the quality of your life.
MPH, U of M Institute on Community Integration
I am a highly motivated, analytical public health advocate with strong interpersonal communication skills. I strive to advance in community health promotion.
MD | he/him/his
Professor | Mayo Clinic Alix School of Medicine
Consultant | Mayo Clinic | Department of Pediatric and Adolescent Medicine | Division of Child Abuse Pediatrics | Mayo Clinic Center for Safe and Healthy Children and Adolescents
MA, LPC, LADC- Women Services Programs at the Department of Human Services, Behavioral Health Division.
I am a doctoral student, experienced Mental Health and Substance Use Disorder Counselor with a demonstrated history of working in the mental health care industry. I’m skilled in Substance Use Disorders, Culturally responsive care, Spanish, Mental Health Counseling, and Community Outreach. I am a healthcare services professional with a Master of Arts – MA focused in Co-Occurring Mental Health and Substance Use Disorder.
Essentia Health
Lead Neonatal Nurse Practitioner in Duluth, MN for the past 25 years.
MD, Children’s
Erin is a neonatologist at Children’s Minnesota. She completed her pediatric residency and neonatology fellowship at the University of Minnesota. Dr Plummer specializes in neonatal critical care at Children’s Minnesota. She is originally from Ohio and attended medical school at Wright State University Boonshoft School of Medicine in Dayton, OH. She completed her residency and fellowship at the University of Minnesota Medical Center. Her clinical interests include nutrition, growth, and neurodevelopmental outcomes in premature and critically ill infants. She is passionate about caring for infants hospitalized in the NICU and building relationships with their families. Dr Plummer is involved in the education of neonatal fellows, pediatrics residents, family practice residents and medical students. She lives in Minneapolis with her husband and two children.
University of Minnesota
Erin Morris is a Neonatal-Perinatal medicine fellow at the University of Minnesota. Her research interests include nutrition and neurodevelopment of infants in the NICU and specifically of those with prenatal drug exposures. She is currently involved in a QI project through the University of Minnesota involving the implementation of the Eat, Sleep, Console treatment for infants with prenatal opioid exposures.
MD, Hennepin Healthcare
Frances Prekker, MD is a Pediatric Hospitalist with Hennepin Healthcare. She is the Medical Director of both the Newborn Nursery and Pediatric Inpatient Unit at Hennepin County Medical Center. She has a special interest in the care of substance-exposed newborns, perinatal substance use, and providing care that preserves the mother-infant dyad. She has led many QI projects at HCMC improving care for infants experiencing withdrawal, keeping moms and babies rooming in together, and reducing bias in newborn drug testing.
Ph.D., University of Minnesota
Jennifer Hall-Lande, Ph.D., is a Psychologist and Research Associate at the Institute on Community Integration (UCEDD) at the University of Minnesota. Dr. Hall-Lande does clinical work in child development, including early identification of Autism Spectrum Disorder (ASD) and other neurodevelopmental disabilities. She is also a former LEND (Leadership in Neurodevelopmental Disabilities) Fellow and remains actively involved as a faculty mentor in the Minnesota LEND program.
MD, MNPQC Board President, MHealth Fairview
Dr. Jessica L. Nyholm is an obstetrician-gynecologist in Minneapolis and is affiliated with multiple hospitals in the area, including M Health Fairview, University of Minnesota Medical Center, and Maple Grove Hospital. She began as a specialist in Maternal-Fetal Medicine at the University of Minnesota. Jessica is passionate about Quality Improvement in Obstetrics, with involvement in both the OB Clinical Practice Council through North Memorial Health and Zero Birth Injury (ZBI) through M Health. Additionally, she has an interest in perinatal infections, with a focus on cytomegalovirus infection in pregnancy.
MD, Native American Community Clinic
As a physician serving the Native American Community in Minneapolis, Dr Rabie is passionate about addressing the significant health disparities that impact Native Americans in Minnesota. To address these disparities she became buprenorphine waivered, and pursued specialty in Addiction Medicine. She is also passionate about educating the next generation of physicians to provide care to the Native Community in the context of community medicine. She provides care using the lens of harm reduction.
LMFT, Private Practice
Kelcee currently works in a private practice setting with special training in maternal mental health specifically perinatal mood and anxiety disorders.
She also works in Adult Mental Health as a county case manager, previously working in child protection as well. She has a variety of experiences within rural communities.
Laura Newton is the Program Director at the Indian Child Welfare Act. She holds a Bachelor of Science in Social Work from Augsburg University.
Minnesota Department of Human Services
Megan is a benefit policy specialist at the Department of Human Services. Her focus is on benefit coverage criteria for Minnesota Health Care Programs which covers Medicaid and MinnesotaCare. She has a doctorate in Occupational Therapy from St. Catherine University and a Masters in Science in Human Services from Capella University. Her goal is to eliminate disparities in health care coverage through policy change.
DNP, APRN, CNM, University of St. Thomas
Meagan Thompson, DNP, APRN, CNM, has a BA in Sociology from the University of Wisconsin Madison in Sociology, with minors in American Indian Studies and Women’s Studies. She worked as a reproductive health educator before returning for her Masters of Nursing (MN) at the University of Minnesota-Twin Cities. In her role as a reproductive health educator, she created educational content to engage young people in their social, emotional, and reproductive health in a variety of settings. After receiving her MN degree, Meagan worked as an RN in a high-acuity tertiary care labor and delivery unit. While working as a bedside nurse, Meagan pursued her Doctorate of Nursing Practice (DNP) degree in the Nurse-Midwifery specialty. During her DNP program, Meagan participated in the Leadership Education in Adolescent Health (LEAH) Fellowship. She worked as part of an interdisciplinary cohort to learn the basics of research, grant writing, and interprofessional collaboration. Her fellowship project examined reproductive outcomes for incarcerated adolescents. Meagan is currently enrolled in a Psychiatric Mental Health Nurse Practitioner (PMHNP) certificate program through the University of Iowa. Upon graduation, she will be a dual-certified CNM/PMHNP provider uniquely qualified to care for perinatal substance use disorders. After graduation from the DNP program, Meagan worked at the University of Iowa where she received funding to implement universal SBIRT and create a maternal substance use disorder (MSUD) clinic. She worked as the primary provider in the MSUD clinic before returning to MN.
Samantha Sommerness, DNP, APRN, CNM
Samantha Sommerness is a Clinical Associate Professor at the University of Minnesota’s School of Nursing. She has expertise in Midwifery, Child, and family health. She has received many accolades, including publications in numerous journals.
Tri-County Health Care
RN, BSN, IBCLC, CPST
Sarah is the OB Supervisor of a critical access hospital in Midwestern Minnesota. She has been married to her husband Nathan for 28 years. They live on a farm with beef cattle and pigs, and have 3 children- Daniel is 23, Megan is 18, and Abby is 16. Sarah has worked at TCHC for 28 years, first as a CNA, then LPN, then RN, BSN, IBCLC, and finally OB Supervisor.